About Jaw Surgery And Why To Avoid It
Orthognathic surgery—commonly called jaw surgery—is often presented by surgeons as a safe, corrective procedure to improve facial alignment, bite function, and appearance. The reality is more complex, and in many cases, far more dangerous than patients are led to believe. This is not a minor dental adjustment—it is a major, invasive operation that permanently alters your jaw, teeth, nerves, and overall facial structure. The decision to undergo jaw surgery should never be taken lightly, and for most people, avoiding it is the safest and healthiest choice.
On This Page
-
About Jaw Surgery → Jaw surgery is often marketed as corrective and safe, but in reality it is more dangerous than presented.
-
Why It’s Recommended → Surgeons cite bite, sleep, or appearance issues, yet these reasons are often exaggerated or subjective.
-
How It Works → The operation involves cutting and repositioning bones, which permanently alters the face and requires long recovery.
-
The Real Dangers → Complications like nerve damage, chronic pain, relapse, and psychological harm are common and lasting.
-
Alternatives Exist → Braces, therapy, dental adjustments, or simply adapting are far safer paths to function and comfort.
-
Bottom Line → For most people, keeping their natural jaw is healthier and safer than risking surgery’s irreversible harms.
What is Orthognathic (Jaw) Surgery?
Orthognathic surgery is a set of procedures designed to reposition the jaws—upper (maxilla), lower (mandible), or both (bimaxillary surgery). It is typically performed by an oral and maxillofacial surgeon in a hospital setting under general anesthesia. Surgeons cut the jaw bones, move them into a new position, and secure them with plates, screws, or wires. The bones are then left to heal in their altered position over several months.
This is not a cosmetic quick-fix—it is a serious skeletal operation with long healing times, significant nerve disruption, and permanent structural changes.
Quick Facts: Jaw Surgery
Type of procedure: Major bone surgery
Recovery time: 3–12 months for full healing
Common goals: Bite correction, facial symmetry, sleep apnea treatment, cosmetic changes
Reality check: High risk of chronic pain, nerve damage, and worsened function
Alternatives: Braces, myofunctional therapy, TMJ physical therapy, cosmetic dentistry, no action
Why Do People Get Jaw Surgery?
Patients are usually told they need orthognathic surgery for one or more of the following reasons:
Bite problems (malocclusion)—overbite, underbite, crossbite
Facial asymmetry or disproportion
Speech difficulties attributed to jaw position
Chewing and swallowing issues
Sleep apnea (in severe cases)
Cosmetic concerns about facial profile or symmetry
While these reasons can sound medically compelling, in many cases they are based on subjective aesthetic judgments or mild functional issues that can be addressed with far less invasive methods or simply lived with.
Who Gets Jaw Surgery?
Jaw surgery is typically recommended for teenagers and young adults once facial growth is complete, since operating earlier could be undone by continued bone development. It is most often considered for people with significant bite misalignments—such as severe overbites, underbites, or crossbites—that orthodontics alone cannot fully correct. Many patients are referred by orthodontists during or after braces treatment. Others pursue the procedure primarily for cosmetic reasons, seeking improved facial proportions, symmetry, or overall balance in their appearance.
How is Jaw Surgery Performed?
A typical jaw surgery procedure involves:
General anesthesia—you are completely unconscious.
Bone cutting (osteotomy)—the surgeon saws through one or both jawbones.
Bone repositioning—moving the jaws to a new angle or location.
Fixation—metal plates and screws are driven into the bones to hold them in their new place.
Jaw surgery is often described as a “routine procedure,” but in reality, what your body experiences is closer to a violent accident than a harmless correction. Your jawbones are deliberately fractured with surgical saws, forced into new positions, and bolted together with metal screws and plates—just as if your face had been shattered in a car crash and pieced back together. Just because a surgical cut is done intentionally does not make any difference to the body. To the body, this is not healing but controlled trauma: bones broken, nerves damaged, pain and disruption of function forever. Even if doctors present it as safe or clinical, nothing can erase the fact that this is a brutal, deconstruction and reassembly of your skull, and the seriousness of that violence should never be minimized.
 Thinking About Jaw Surgery? Read This First.
Thinking About Jaw Surgery? Read This First.
Orthognathic surgery is not a harmless tune-up. It is major bone surgery with permanent consequences:
Once the surgery happens, can’t “Change your mind” and go back in time if things don’t turn out.
Nerve damage is common—and often irreversible.
Many patients report worse chewing, speaking, and pain afterward.
Some never feel comfortable with their new face.
Depression and regret are more common than surgeons admit.
Bottom line:
If your issue isn’t life-threatening, the safest choice is often to keep your natural jaw. Your health, comfort, and quality of life will thank you.
The Dangers of Jaw Surgery
Orthognathic surgery carries serious, life-altering risks that are often downplayed in consultations. These include:
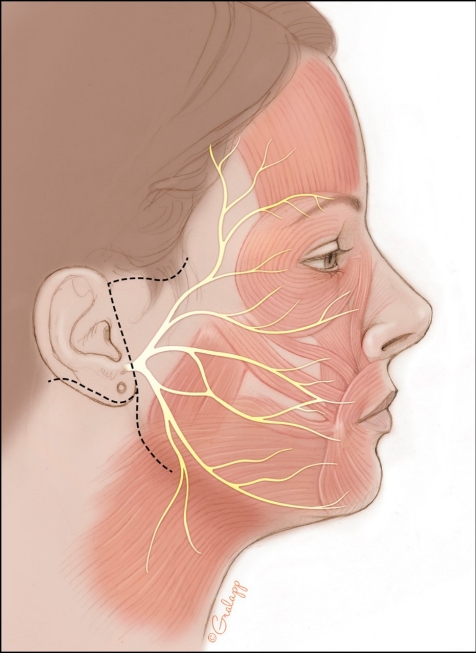
Permanent nerve damage (numbness, tingling, burning pain) in lips, cheeks, or tongue
Chronic jaw pain and temporomandibular joint disorder (TMD)
Difficulty chewing and swallowing—sometimes worse than before surgery
Speech impairment
Relapse — jaws shift back toward original position, undoing results
Infection and bone healing problems
Mental health decline — depression, anxiety, regret, body image distress
Loss of bite strength and stability
Altered facial identity that feels unnatural or uncomfortable
These outcomes are common because the face is not a simple structure that can be altered without consequences—it is one of the most complex, sensitive, and highly integrated regions of the human body. The jaws are surrounded by a dense network of sensory nerves, muscles, joints, and soft tissues that all work together for vital functions like eating, speaking, and expressing emotion. Cutting through bone and shifting it into a new position inevitably disrupts this delicate system. Even when the surgery is technically “successful” by medical standards, the body often struggles to fully adapt to the new arrangement, leaving patients with pain, dysfunction, or sensory loss.
The face is also central to identity and emotional well-being, which makes complications especially difficult to cope with. Unlike other surgeries, jaw surgery permanently alters both form and function in a highly visible area tied to how you look, feel, and interact with the world. Because nerves in the face are so densely packed and finely tuned, even small injuries can cause disproportionate, lasting effects such as burning pain, altered sensations, or facial asymmetry. Combined with the mechanical stress placed on the jaw joints and muscles after repositioning, it is easy to see why long-term complications are not rare accidents, but rather an expected risk when such a vital, nerve-dense area is surgically altered. While some patients do experience functional improvement, the proportion who develop lasting problems is high—and these problems are often far worse than the initial issue.
Even a few leading experts within the field have openly acknowledged these limitations. Professor William Bell — often referred to as the “Godfather of orthognathic surgery” for his prolific research, textbooks, and influence — at the end of his career famously described jaw surgery as “too complicated, too invasive, too time-consuming, too expensive and too unpredictable.” Coming from one of the most respected authorities in oral and maxillofacial surgery, this statement underscores just how inherently risky and uncertain the procedure is. If the very pioneer of the field warned of its complexity and unpredictability, it raises serious questions about why patients are still being told it is routine, safe, and reliable.
Alternatives to Jaw Surgery
For most people, safer options exist:
Doing nothing at all — In some cases, the best option is simply to avoid unnecessary intervention. Many so-called “problems” identified by surgeons are within the range of natural variation and do not cause serious health issues. Attempting to “fix” them surgically may create new problems far worse than the original concern. Accepting one’s natural bite and appearance is often safer, less stressful, and a better long-term choice than undergoing a high-risk, irreversible operation.
Orthodontics (braces or clear aligners) — Traditional braces and modern clear aligners like Invisalign can correct a wide range of bite problems, including crowding, spacing, overbites, underbites, and crossbites. While they cannot move the actual bone structure of the jaw, they are often sufficient to bring teeth into closer alignment, improving both appearance and function. Orthodontics works gradually by applying gentle, controlled pressure to teeth, shifting them into healthier positions over time. Many people who are told they “need surgery” find that orthodontic treatment alone provides excellent results without the risks of cutting and repositioning bone.
Myofunctional therapy — This is a specialized exercise program designed to retrain the muscles of the tongue, lips, and face. It can be especially helpful for people with open bites, tongue-thrusting habits, or jaw tension that contributes to misalignment and breathing issues. By strengthening and re-patterning oral muscles, myofunctional therapy improves the natural balance of the face and jaw. It is non-invasive, can be done at home under professional guidance, and often works best in combination with orthodontics for long-term stability.
Physical therapy for TMJ — Many jaw surgery candidates struggle with temporomandibular joint (TMJ) pain, clicking, or restricted movement. Physical therapy can reduce these symptoms without altering the jaw structure. Through techniques such as manual therapy, posture correction, ultrasound, and guided jaw exercises, physical therapists help restore mobility, reduce inflammation, and relieve muscle strain. This approach addresses the functional problems directly, without creating new ones from surgery, and can be repeated or adjusted as needed.
Dental prosthetics — Sometimes bite issues are not due to the jaw at all, but rather to the shape, size, or wear of individual teeth. In these cases, dentists can use crowns, veneers, or reshaping (called equilibration) to improve how teeth come together. This can correct minor misalignments, restore bite stability, and enhance smile aesthetics. Prosthetic solutions are far less invasive than bone surgery, and they can be tailored to each patient’s unique dental structure.
Lifestyle changes — For conditions like sleep apnea, jaw tension, or teeth grinding (bruxism), simple lifestyle changes can have a powerful impact. Weight management, better sleep positioning, stress reduction, and oral appliances like mandibular advancement devices can dramatically improve symptoms. These approaches address the root causes of airway or muscle strain problems, instead of surgically altering the jaw and risking permanent damage.
Cosmetic dentistry — When the main concern is appearance rather than function, cosmetic dentistry can provide a safe and effective alternative. Veneers, bonding, gum contouring, and teeth whitening can all improve smile harmony without altering the bone structure of the jaw. Even minor adjustments to tooth size or shape can make a big difference in facial balance and self-confidence.
Facial muscle exercises — Targeted exercises can help improve jaw mobility, strengthen weak areas, and bring greater balance to facial appearance. These exercises may help with mild asymmetry, jaw fatigue, or poor posture contributing to bite issues. Over time, consistent practice can enhance both function and appearance, supporting other non-surgical treatments like orthodontics or myofunctional therapy.
Risks vs. Alternatives
 Risks of Jaw Surgery
Risks of Jaw Surgery
Permanent nerve damage → loss of sensation, burning, tingling in face or tongue
Chronic jaw/TMJ pain → daily discomfort, headaches, reduced quality of life
Speech & chewing difficulties → sometimes worse than before
Relapse → jaw shifting back toward original position
Infections & bone healing problems → long recovery or secondary surgeries
Mental health decline → depression, anxiety, body image distress
 Non-Surgical Alternatives
Non-Surgical Alternatives
Orthodontics (braces, aligners) — corrects bite without bone cutting
Myofunctional therapy — strengthens jaw, tongue, and facial muscles
Physical therapy for TMJ — reduces pain and improves movement
Cosmetic dentistry — veneers, crowns, bonding for smile improvement
Lifestyle & airway changes — improve sleep apnea without surgery
Adaptive strategies — small functional adjustments without high risk
Can You Just Live Without Surgery?
Yes—many people with imperfect bites or asymmetrical faces live full, healthy lives with no functional problems at all. The truth is, perfection is not required for comfort, health, or confidence. The human jaw is incredibly adaptable. Even people with jaw variances are usually able to eat, speak and breathe just fine. Minor functional inconveniences rarely justify the high cost—mentally, physically and emotionally—of jaw surgery.
When to Say “No”
If your jaw issues are mostly cosmetic, mildly functional, or already manageable, surgery often does more harm than good. The safest choice may be to keep your natural jaw and address concerns through less invasive means.
Bottom Line: Why You Should Avoid Jaw Surgery
Orthognathic surgery is often marketed as a path to improved function and beauty, but for many, many, many patients, it leads to chronic pain, worsened function, and long-term psychological harm. If you are being advised to undergo jaw surgery, seek multiple second opinions, research patient outcomes, and employ non-surgical alternatives.
Sometimes, the healthiest and most life-affirming choice is to accept and adapt, rather than submit to a high-risk operation.
Your jaw is not broken — but if you go through with jaw surgery, it quite literally will be.