Why Does Jaw Surgery Cause So Much Pain?
Jaw surgery is often presented as just another medical procedure—an intervention on par with having your appendix removed or a joint arthroscopy. But this framing leaves out something crucial: not all surgeries are equal. Operating on the jaw is uniquely invasive, painful, and disruptive to daily life, and understanding why requires looking at the biology of the face, the mechanics of bone healing, and the constant use of the jaw in everyday activity.
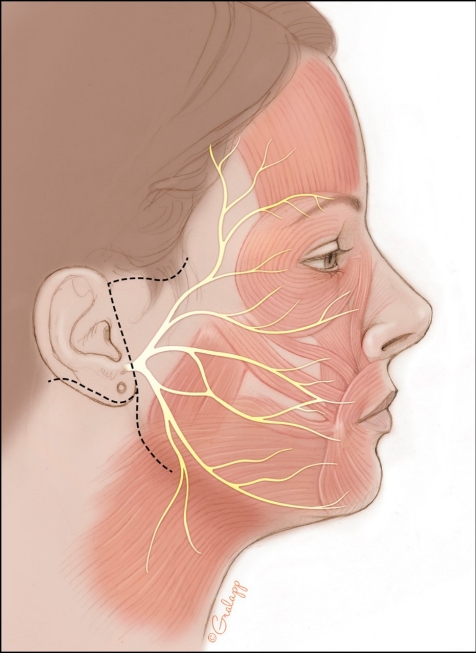
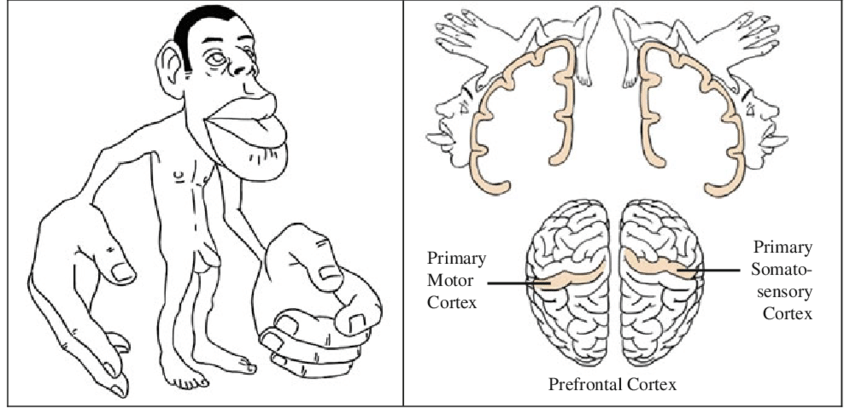
The Face: The Body’s Sensory Hotspot
If you’ve ever seen a homunculus diagram—an image mapping the human body by sensory nerve distribution—you’ll notice one thing immediately: the face and mouth dominate the map. They are the most densely innervated areas of the body. This means that any trauma, incision, or bone-cutting in this region involves enormous sensory input, and with that comes significant pain.
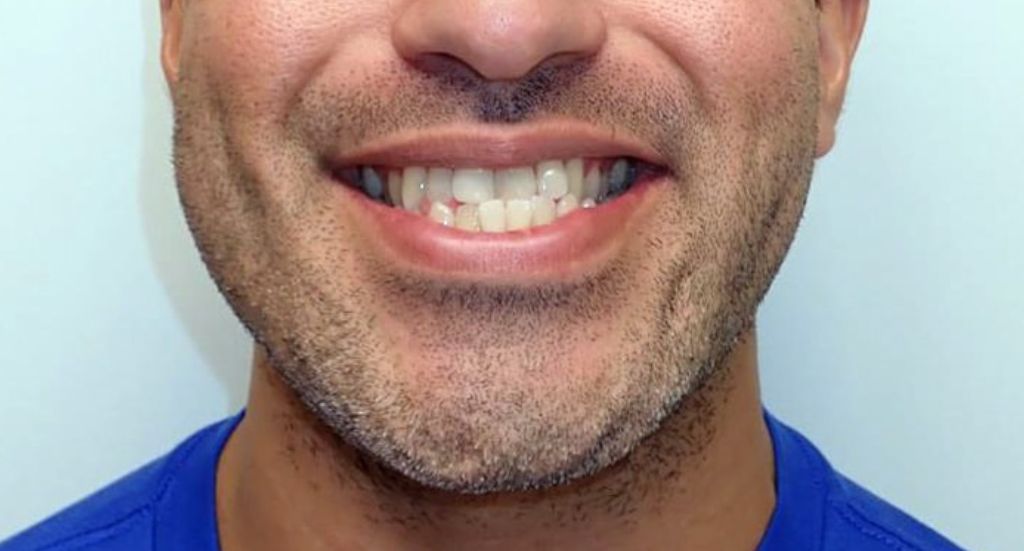
Unlike a knee or a shoulder, your jaw isn’t an area that can be “rested.” Every time you eat, talk, or even swallow, you’re using this region. That constant activity prevents true rest and magnifies discomfort.
Cutting Bone, Not Just Skin
Most people think of surgery in terms of cutting skin or connective tissue. Jaw surgery goes much deeper: it involves sawing through bone—the living, dynamic foundation of your face. Bone is not dead construction material. It is a highly vascularized organ, filled with marrow, nerves, and an interosseous cavity actively engaged in cellular metabolism. Cutting bone is far more traumatic than cutting skin, and the healing process is longer, more painful, and more prone to complications.
Medical literature and news reports often warn that bone surgery carries greater risks of pain and long-term discomfort than many soft-tissue procedures. While arthroscopic knee surgery may involve tiny instruments, minimal scarring, and relatively quick recovery, orthognathic surgery means fracturing and repositioning major facial bones, then asking the body to heal under constant stress.
Titanium Hardware and Irritation
To stabilize the repositioned bones, surgeons typically leave titanium plates and screws in the face. While titanium is considered biocompatible, that doesn’t mean it is always symptom-free. Many surgeries throughout medicine do not involve leaving hardware behind, but in jaw surgery, permanent implants are the norm. For some patients, this hardware becomes a source of irritation, chronic inflammation, or lingering pain—adding yet another layer of discomfort to the recovery.
Changing the Skull’s Mechanics
Your skull and jaw are not just static structures. They are the product of years—decades—of natural adaptation. The way your jaw hinges, the pull of your muscles, and the alignment of tissues across your head are finely tuned to your unique anatomy. When surgery changes the distal end of the jaw, the entire system must readapt.
The jaw joint must accommodate new angles of stress.
Muscles that once pulled along familiar paths must now adjust to different lengths and directions.
Areas of compression and tension arise where tissues are not conditioned to handle them.
This mechanical disruption can create lasting soreness, joint discomfort, and muscle fatigue.
Bone Healing and Scar Tissue
Surgery Is Not All The Same
Key Reasons Jaw Surgery Is More Painful Than Most Surgeries
| Factor | Why It Makes Jaw Surgery Painful |
|---|---|
| Sensory-rich facial nerves | Small injuries register as extreme pain |
| Bone trauma | Living bone heals slowly and painfully |
| Titanium hardware | May irritate and require later removal |
| Mechanical disruption | Muscles/joints forced into new patterns |
| Nerve damage & scar tissue | Risk of chronic pain or numbness |
| No rest possible | Jaw is in constant daily use |
While some surgeries are quick and low-risk, jaw surgery belongs in a category of its own: high-trauma, high-pain, and life-disrupting.
In Summary
Jaw surgery causes so much pain because it combines several uniquely challenging factors:
-
Operating in the most nerve-dense region of the body.
-
Cutting through living bone rather than soft tissue.
-
Leaving hardware behind that can trigger irritation.
-
Forcing constant use of the healing site.
-
Altering the finely tuned mechanics of the skull and jaw.
-
Risking nerve damage, scar tissue, and maladaptive healing responses.
This is not the same as a “routine surgery.” It is an invasive alteration to one of the most complex and sensitive systems in the human body. Pain is not an outlier—it is a defining feature of the procedure.